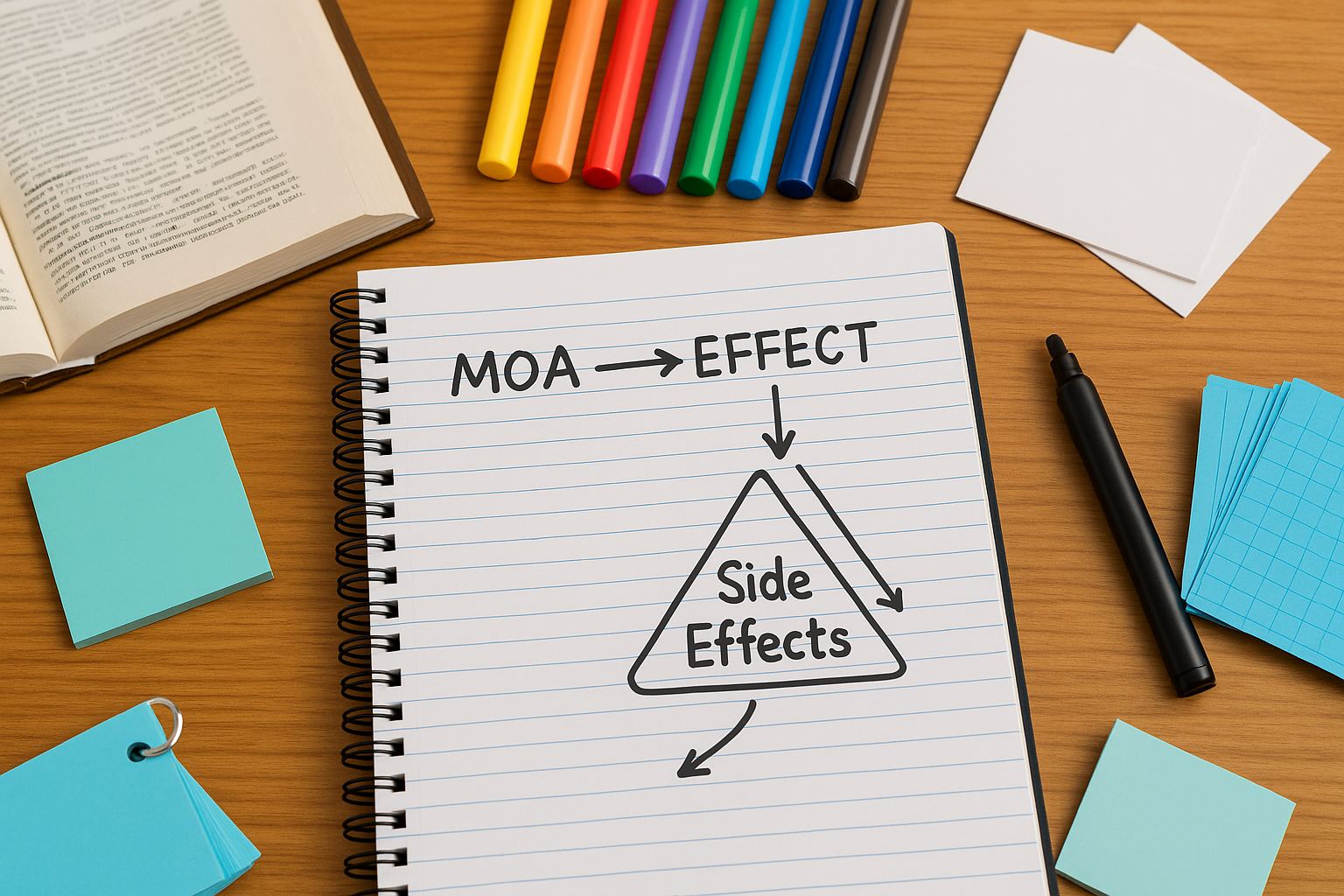
Pharmacology overwhelms because it looks like an index of isolated facts—names, mechanisms, indications, toxicities. The reflex is to reach for cute, one-off mnemonics. Yet shallow wordplay rarely survives exam conditions: it doesn’t bind meaning, it doesn’t connect to prior knowledge, and it fails under stress. Effective memory systems do the opposite. They convert lists into meaningful structures, then strengthen those structures with retrieval practice, spaced repetition, dual coding (verbal + visual), and interleaving. The outcome you want isn’t “remembering the line” — it’s recognizing patterns and reconstructing answers when the stem is novel. Start with anchor drugs — a representative member of a class whose mechanism and toxicity you know cold. Build outward with mechanism-based logic: if a drug increases serotonin, what improves, what worsens, and what synergizes? This creates cause–effect threads that hold even when names blur. Then, apply active recall: quiz yourself before re-reading. Testing is not just an “assessment” step — it’s the learning event. Next, schedule reviews using a spacing algorithm aligned with the forgetting curve; you should revisit right before performance erodes, not after you’ve fully forgotten. Finally, interleave content (e.g., beta-blockers mixed with ACE inhibitors and diuretics) to improve discrimination — the exact skill Step 1 demands when two choices feel plausible. MDSteps operationalizes this system: our Adaptive QBank (9000+ questions) triggers retrieval under exam-like conditions; our automatic flashcard decks are generated from your misses and weak topics and are exportable to Anki; our analytics and readiness dashboard recommends spacing intervals by topic and maps which mechanism clusters slip fastest. With these tools, mnemonics stop being fragile tricks and become hooks embedded in a durable network you revisit, test, and refine. A good pharmacology mnemonic is diagnostic: it helps you decode new stems by mechanism, not just recite lists by rote. Use these design rules: Build your mnemonic in a two-directional format: (A) given the drug, retrieve the mechanism and AE; (B) given the tox pattern, retrieve likely classes. Practice both directions deliberately. In MDSteps, create two flashcards per anchor — forward (name → MOA/AE) and reverse (tox pattern → class/name) — or let the platform auto-generate them from your QBank explanations. Use image fields to store a single sketch that encodes the pathway; avoid clip-art clutter. Finally, standardize tags so your decks are sortable by system (CV, renal, neuro), mechanism (receptor/pathway), and tox pattern (e.g., cholestasis, torsades, photosensitivity). MDSteps’ automatic study plan generator pulls these tags into weekly blocks and interleaves adjacent mechanisms to sharpen discrimination. The literature is consistent: durable learning emerges from retrieval practice and spacing, amplified by dual coding — using both verbal propositions and visual representations. For pharm, that means pairing minimal text (MOA, indications, AEs) with a meaningful schematic: receptor → second messenger → organ response. Peg systems (number–image hooks) can help with small fixed lists (e.g., CYP inducers/inhibitors), but become unwieldy for sprawling classes unless tied back to mechanism maps. Narrative mnemonics work when the story mirrors causality; cute puns detached from physiology fade quickly. Implement dual coding with a standard template: a thumbnail pathway diagram plus one color-coded “tox triangle” listing the three highest-yield adverse effects. Keep graphics spartan. Over-decoration reduces transfer. In your flashcards, place the image on one side and ask for the MOA/AE set on the other (or vice versa). This forces cue utilization from both channels. MDSteps supports image-backed cards and tracks which image prompts yield faster correct responses. If an image doesn’t accelerate retrieval by week two, replace it. Our analytics surface underperforming cards, suggesting edits or swaps and recalculating spacing based on your accuracy/latency. Over time, you cultivate a lean visual lexicon — a set of reusable icons and arrows you instantly parse during a stem. Bottom line: fuse mechanism diagrams with crisp verbal prompts; reserve narrative or peg systems for bounded sets; retire anything that doesn’t measurably speed recall. Let data steer the art. Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data. Spacing works when intervals are just long enough to make retrieval effortful but successful. Here’s a practical 30-day loop for Step 1 pharm anchors (assumes daily 45–60 minutes of pharm review alongside systems work): MDSteps automates the schedule. The readiness dashboard predicts when each mechanism cluster will slip below 80% and surfaces those cards for review; the AI tutor can rewrite leech cards into shorter, mechanism-first prompts. Export to Anki if desired; your intervals sync via tags and due dates. Most Step 1 misses happen not because you “don’t know” pharm, but because two options seem reasonable and you can’t discriminate. Interleaving fixes that by forcing side-by-side comparisons during practice. Rather than drilling all ACE inhibitors, build sets that pit ACE inhibitors vs. ARBs vs. direct renin inhibitors, or β1-selective vs. nonselective β-blockers with partial agonism. This creates contrastive features — the exact cues you’ll need when a stem hints at cough/angioedema (ACE) or hyperkalemia in CKD (ACE/ARB) or bradycardia in an asthmatic (prefer β1-selective). Structure a 20-minute block as follows: (1) 6–8 interleaved cards (reverse direction first: tox pattern → class); (2) one 10-question timed QBank set containing mixed cardio-renal pharm; (3) a 3-minute “error anatomy” review where you write one if-then discriminator per miss (“If diabetic with albuminuria → ACE/ARB for renal protection”). Tag each discriminator into your deck as a microcard. MDSteps’ adaptive QBank can auto-compose mixed sets targeting your confusable pairs and track nearest neighbor errors (which wrong option you choose most often). The system then generates contrast cards that present the two mechanisms and ask for the single feature that separates them. Over a week, error gravity shifts from “these both look right” to “only one fits the mechanism trail.” Measure success by latency as well as accuracy. If you’re correct but slow, add a one-image cue (e.g., bradykinin cloud for ACE inhibitors) and review it at short intervals until response time drops. Decision speed is learnable — and graded by the clock on exam day. Use this matrix to pick the right mnemonic for the job. Keep it lean; swap anything that doesn’t speed recall. MDSteps’ AI tutor can convert your verbose notes into mechanism maps and contrast cards automatically, then push them into your daily queue. If a mnemonic doesn’t reduce errors or latency within one week, the dashboard flags it for revision. Treat your toolkit as living — ruthlessly simple, relentlessly tested. Every miss is a design brief for a better mnemonic. Convert errors into targeted prompts within 5 minutes of finishing a set. Workflow: (1) do a 10–20 question timed set; (2) for each miss, extract the single causal link you overlooked (“non-dihydropyridine CCBs → ↓AV nodal conduction → bradycardia/heart block”); (3) create one reverse card (“Elderly with constipation, bradycardia after starting antianginal → which class?”); (4) sketch a tiny mechanism arrow graphic; (5) schedule an early review (24–48 hours); (6) interleave with its confusable neighbor class in the next session. MDSteps handles steps 2–5 for you: explanations auto-generate forward + reverse flashcards with the key discriminator bolded, place them in a short-interval review bucket, and recommend a confusable pair for your next set. The readiness dashboard visualizes which discriminators still leak points. Use that heatmap to pick tomorrow’s interleaved pairings. Within a week, your personal mnemonic library mirrors your error profile — exactly what Step 1 pressures. Keep cards atomic. If a card contains more than one mechanistic leap, split it. Tag each with Mnemonics earn their keep only if they collapse decision time under pressure. Two weeks out, shift toward simulation blocks: 40–80 mixed questions in timed mode, strict pacing (≈90 seconds per item), and a post-block forensic. For each question, label which cue triggered selection (mechanism arrow, tox triangle, anchor variant). Track two metrics: first-pass accuracy and mean decision latency. If your accuracy is ≥80% but you’re slow, create micro-images (one icon per discriminator) and rehearse them in short-interval bursts. If accuracy lags, revise the underlying mechanism map — not the wordplay. Build an Exam-Day Essentials routine: (1) five contrasting pairs you historically confuse; (2) 12 anchor cards (forward + reverse) across three systems; (3) three mechanism diagrams you want at your fingertips (e.g., RAAS, adrenergic pharmacology, arachidonic acid pathway). Review them the night before and the morning of the exam — no new content. This primes the exact retrieval routes Step 1 exploits. MDSteps streamlines this phase. The automatic study plan generator builds a taper that increases mixed timed sets while ratcheting review volume down, preserving freshness without fatigue. The analytics dashboard turns your last seven days of errors into a one-page “Final Five” discriminators list. Carry that list into your final two rehearsals; if it stops generating errors, you’re ready. Remember: your goal isn’t to memorize every drug equally. It’s to master mechanistic anchors and discriminators — the compact set of cues that unlock most Step 1 items. With a lean mnemonic library, spaced reviews, and relentless interleaving, you’ll convert pharm from panic to pattern. Why Most Pharm Mnemonics Fail (and How to Make Them Work)
Design Rules for High-Yield Mnemonics
Dual Coding, Peg Systems, and Narrative Imagery — What the Evidence Supports
Master your USMLE prep with MDSteps.
100+ new students last month.
Spaced Repetition Scheduling — A 30-Day Template You Can Actually Follow
Weeks 1–2 (Encoding & Calibration)
Weeks 3–4 (Consolidation & Discrimination)
Interleaving & Discrimination: Training Yourself to Pick the Right Similar Answer
A Compact Toolkit of Mnemonic Types (and When to Use Each)
Type Best Use Case Design Tips Pitfalls Mechanism Map Link receptor/pathway → organ effect → AE 1 diagram + 3 “tox triangle” bullets Overdecorating; losing causal arrows Anchor + Variants Class with many look-alikes Pick 1 archetype; contrast key variants Memorizing all names equally Narrative Cue Small sets (e.g., isoniazid AEs) Story must mirror physiology Forced puns unrelated to mechanism Peg List CYP inducers/inhibitors; Teratogens Limit to ≤10 items; refresh often Scales poorly; interference Contrast Card Interleaving confusables Ask for the single discriminator Too many features per card From QBank Misses to Superior Mnemonics — A Closed-Loop Workflow
system, mechanism, and tox. Atomicity increases successful retrievals, which amplifies spacing efficiency. Your goal isn’t bigger decks; it’s sharper cues with measurable impact on decision speed.
Exam-Day Simulation: Turning Mnemonics into Fast, Mechanistic Decisions
References & Further Reading
Mnemonic Medicine: Evidence-Based Memory Systems for Step 1 Pharmacology