Why a 30-Day Plan Works on Rotations: Constraints, KPIs, and Guardrails
Thirty days is long enough to build pattern recognition and short enough to maintain intensity on service. The goal isn’t encyclopedic coverage; it’s decision speed on common inpatient and ambulatory problems. We anchor the month to three KPIs: question throughput (≥1,200 mixed clinical vignettes), retention yield (measured via spaced “hot list” items mastered), and readiness trend (practice-form trajectory with realistic confidence bands). These KPIs map to learning-science pillars: the testing effect (retrieval trumps reread), spaced repetition (durable memory with short, frequent passes), and interleaving (mixed domains sharpen discrimination under time pressure).
Rotations add constraints: post-call fatigue, pages, unpredictable procedures, and documentation. Therefore, the plan is built around time-boxed sessions you can deploy in 20–40 minute windows and a nightly rapid review that tops out at 25–30 minutes. We also enforce Friday slack—a built-in 10–15% buffer for life and service volatility—so the schedule doesn’t collapse after one bad week. Finally, we avoid cognitive overload by separating performance (timed blocks) from deliberate practice (slow, mechanism-first review) and by using a standardized error script so difficult cases convert into rules you’ll apply on exam day.
- Daily floor: 40–60 mixed questions (timed), even post-call (minimum 20).
- Review cap: 90 minutes on full days; 30 minutes post-call; defer deep dives to weekend.
- Practice cadence: diagnostic on Day 1 (baseline), progress check on Day 14, decision check on Day 24, dress rehearsal on Day 27.
- MDSteps tools: KPI tracker, incorrects pipeline, and rapid-review checklist templates embedded below.
Your job is to protect the floor, respect the caps, and let the pipeline do the compounding.
Calendar Architecture: Four Weeks That Survive Call and Clinic
Design the month like a service schedule: heavy weekdays, light post-call, strategic weekends. Each weekday has a core block (timed questions) before or after your shift, a micro-block you can do on your phone (2–4 rapid cards), and a review block at home. Weekends run longer, integrating deep review and a mixed diagnostic set. The sequence repeats across four weeks with slightly different emphasis (breadth → weakness targeting → consolidation → taper).
| Week | Focus | Weekday Target | Post-Call Target | Weekend Target | Outcome Metric |
|---|---|---|---|---|---|
| 1 (Days 1–7) | Breadth + Baseline | 40–60 Q/day (timed) | 20–30 Q + 20-min review | 120–160 Q + baseline review | Baseline score; initial hot list |
| 2 (Days 8–14) | Weakness Surfacing | 60 Q/day | 30 Q + tagged incorrects | 160–200 Q + systems pass | Midpoint check (Days 13–14) |
| 3 (Days 15–21) | Mechanism & Rules | 60–80 Q/day | 30 Q + rule-writing | 200 Q + algorithm drills | Rule bank >= 60 entries |
| 4 (Days 22–30) | Refine & Taper | 40–60 Q/day | 20–30 Q + rapid cards | Dress rehearsal + light review | Stable prediction interval |
Place practice forms on Days 1, 14, 24, and 27. Day 1 calibrates; Day 14 verifies slope; Day 24 informs the final 72-hour plan; Day 27 is a dress rehearsal with exam-day settings (breaks, pacing, nutrition). Build Friday slack by scheduling 10–15% fewer questions than your ceiling; use that space to catch up or to protect recovery after tough calls. If you miss a target, never raid sleep; redistribute into Friday or Saturday morning.
Daily Engine: Mixed Timed Blocks + a Tight Incorrects Workflow
The highest ROI comes from mixed, exam-length blocks under time pressure. Run 40–60 questions in timed mode (no tutor) with 90–105 seconds per item. Immediately after, execute a two-stage review. Stage A (fast): mark only items with diagnostic value—true uncertainty, lucky guesses, and conceptual misses—then log the why (knowledge gap, misread, premature closure, or anchoring). Stage B (deep): for the 8–12 most instructive items, write a one-sentence decision rule (e.g., “In painless jaundice + Courvoisier sign, next step is contrast CT for pancreatic head mass”). Convert that rule into a flashcard prompt (question stem fragment → next best step) and tag it by system and error type in your MDSteps incorrects pipeline.
MDSteps Incorrects Script (10–12 min)
- Classify error: knowledge vs. reasoning vs. attention.
- Extract trigger phrase(s) from the stem.
- Write the decision rule (if/then, next best step).
- Link mechanism (1–2 lines) to the rule.
- Create a review card & schedule spaced revisit.
Time Caps That Prevent Slog
- Weekdays: 60–90 min review cap per full block.
- Post-call: 20–30 min max; defer deep dives.
- Weekend: 2× depth on top 10 misses.
Avoid “museum tours” of explanations. Chase transfer: Would your rule change the next similar question? If yes, keep it. If not, archive it. When fatigued, prioritize next-step and management ladder items over esoterica.
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
Content Consolidation: Rapid Review That Actually Finishes
On busy services, note bloat kills momentum. Consolidation should be brief, structured, and scheduled. Use a three-layer system: (1) Rules (your one-liners from incorrects), (2) Algorithms (management ladders for chest pain, GI bleed, stroke, sepsis, prenatal care), and (3) Microfacts (tight numeric anchors like Na⁺ correction rates, steroid stress-dose thresholds, or GAD-7 cutoffs). Your nightly rapid review cycles 6–10 rules, 1–2 algorithms, and 6–10 microfacts in 25–30 minutes.
MDSteps Rapid Review Pipeline (25–30 min cap)
- 5 min: Resurface yesterday’s “due” rules (spacing).
- 10–15 min: New rules from today’s blocks (interleaved).
- 5–7 min: One algorithm rehearsal (say-it-out-loud steps).
- 2–3 min: Microfacts lightning round (numeric anchors only).
Tip: Keep cards terse and recognition-proof. Stem fragment → action. Ditch paragraphs; use verbs and thresholds.
Weekend consolidation adds a systems pass without abandoning interleaving. Do a 60–90 minute walk-through of the highest-weight domains (medicine, OB/GYN, pediatrics, surgery, psychiatry) using mixed question sets to surface blind spots, then plug them into the rule bank. Resist the urge to build encyclopedias; the exam rewards pattern + next step more than trivia. Finally, track leakage—the handful of rules you repeatedly miss. Give them double spacing and rehearse with oral recall to ensure generative retrieval, not recognition.
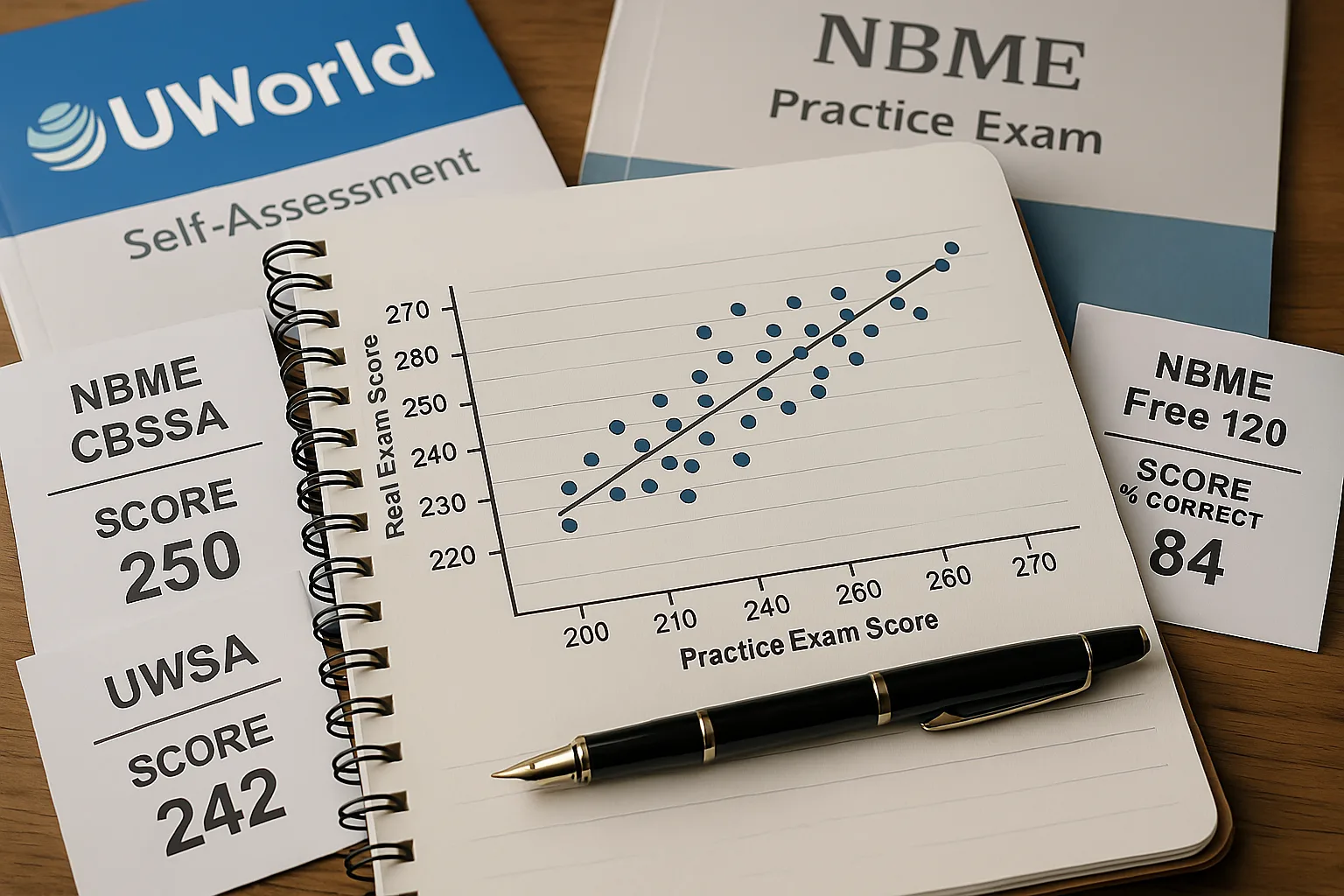
Diagnostics & Decision-Making: Turning Practice Scores into Action
Practice forms are instruments, not verdicts. Each carries both signal (your current level) and error (form difficulty, test-day variance). Treat every result as a range, not a point. Compute a conservative prediction interval by subtracting 5–8 points from your form score to define a floor for planning; if multiple forms cluster, weight the median. Look beyond the total: domain bands (e.g., cardiovascular, respiratory, renal), task types (diagnosis, next step, ethics), and error taxonomy (knowledge vs reasoning vs attention) dictate the next 72 hours of work.
Score → Action Framework
- Baseline (Day 1): Set starting range; identify 3 weak domains.
- Midpoint (Day 14): Check slope. If flat or negative, trim passive reading and add a second mixed block daily for five days.
- Pre-decision (Day 24): If your conservative floor is at or above your target band, proceed; if not, add a 7–10 day micro-extension focused on the top two deficits.
- Dress rehearsal (Day 27): Simulate breaks and pacing; finalize logistics and nutrition plan.
Interpretation note: Consistency across forms beats one high flyer. Outliers are often noise.
Common Pattern Flags
- Low diagnosis, normal management: Add differential drills with triage cues.
- Normal diagnosis, low next step: Rehearse algorithms aloud; build ladder cards.
- High omissions/marked items: Work on pacing (90-sec rule) and first-pass elimination.
Finally, make domain sprints tiny and tactical (e.g., “OB third-trimester bleeding: 30 mixed questions + 3 rules + 1 algorithm”). Ship outcomes within 24 hours, then return to mixed sets to protect transfer.
What to Study First: High-Yield Domains and How to Weight Them
Step 2 CK emphasizes common inpatient and ambulatory scenarios where recognition and management speed matter. Rather than chasing exact percentages (which fluctuate across forms), anchor your time to a pragmatic weighting: Internal Medicine (broad adult care) as the backbone; OB/GYN and Pediatrics for age- and pregnancy-specific algorithms; Surgery for perioperative and trauma management; and Psychiatry/Ethics for safety, capacity, and consent. Within each, prioritize next best step ladders, red-flag triage, and numeric thresholds likely to change management.
| Domain | Pragmatic Emphasis | Core Algorithms to Rehearse | Numeric Anchors |
|---|---|---|---|
| Internal Medicine | High | Chest pain, GI bleed, DKA/HHS, sepsis bundle, AKI | Troponin deltas, MELD/Child-Pugh cues, MAP goals, Na⁺ correction |
| OB/GYN | Moderate-High | Third-trimester bleeding, hypertensive disorders, labor management | Severe-feature BPs, MgSO₄ dosing, RhIg timing |
| Pediatrics | Moderate | Fever in <28/29–60/61–90 days, asthma exacerbation, dehydration | Weight-based fluids, bronchodilator escalation, bilirubin thresholds |
| Surgery/Emergency | Moderate | Abdominal pain triage, trauma primary survey, periop abx/anticoag | Transfusion triggers, hemodynamic targets, NPO windows |
| Psychiatry/Ethics | Moderate | Suicide risk, capacity, involuntary hold, confidentiality exceptions | Screen thresholds (e.g., PHQ-9 bands), criteria snippets |
Spend the first 10 days slightly overweighting Internal Medicine while keeping daily interleaving across OB/GYN, Pediatrics, Surgery, and Psychiatry to maintain discrimination. As weaknesses surface, reallocate 20–30% of daily volume toward those domains for three-day sprints, then return to mixed blocks. Keep a living Numeric Anchors card list; the step from “consider” to “do” often hinges on a range or cutoff.
On-Service Tactics: Studying Through Fatigue, Call, and Clinic
Clinical days drain willpower; design friction-proof habits. Morning micro-set: 6–8 questions on your commute or pre-rounds coffee to prime retrieval. Mid-day reset: if you get 10 minutes, rehearse 3–5 rule cards, not social media. Post-call protocol: 20–30 mixed questions (timed) to keep rhythm, 20-minute rapid review, then full recovery—no guilt. Protect sleep like a medication with strict dosing and timing; the testing effect collapses without consolidation.
Pacing & Error-Proofing on Timed Blocks
- 90-second rule: If you’re stuck, mark, eliminate obvious distractors, pick the leading hypothesis, move on.
- Red-flag first: Vital instability or airway threat? Choose stabilization before diagnostics.
- Read the last line first: Clarifies the task (diagnosis vs. next step vs. test choice) and prevents explanation tours.
- One-pass elimination: Kill answers that violate the stem’s facts or the algorithm’s sequence.
Use the ward to your advantage. When you encounter a case (e.g., pancreatitis, UGIB, preeclampsia), write a 48-hour mini-sprint: 20 related questions, 3 decision rules, 1 algorithm rehearsal. Discuss the ladder with a senior or attending to sharpen pragmatics. For documentation-heavy days, switch to micro-blocks: three 7-question bursts spaced through the day behave like one 21-question set and keep your streak intact. Finally, prevent erosion by setting a daily shutdown ritual (screen off, tomorrow’s question count set, three wins noted). Momentum beats motivation.
Final 72 Hours, Exam-Day Logistics, and the Rapid-Review Checklist
The last three days convert knowledge into execution. Day −3: two mixed blocks (timed), 60–90 minutes of targeted review, algorithm rehearsal aloud, finalize travel and ID. Day −2: one full mixed block plus a light incorrects sweep; confirm meals, fluids, layers, and break structure. Day −1: half-day only—one 40-question set, 20-minute rapid cards, and a walk; screens off by 7–8 p.m., sleep on schedule. If anxiety spikes, rehearse your first 10 minutes—check-in, locker, earplugs, first passage cadence.
Rapid-Review Checklist (Print or Save)
- Top 30 decision rules (cardiac chest pain, stroke window, sepsis bundle, GIB ladder, DKA/HHS, third-trimester bleed, neonatal fever).
- 10 algorithms said aloud (no notes): ACS, PE, COPD/Asthma exacerbation, AKI, prenatal care by trimester, hypertensive disorders of pregnancy, pediatric fever age-bands, suicide risk, delirium vs dementia, perioperative anticoagulation.
- Numeric anchors: insulin infusion starts, MgSO₄ dosing, Na⁺ correction rates, transfusion triggers, steroid stress dosing, bilirubin phototherapy thresholds.
- Pacing: 90–100 seconds per item with a planned second sweep for marked questions.
- Break plan: fluids every two blocks, protein + complex carbs, brief stretch, eye rest.
- Logistics: ID, confirmation, earplugs/headphones, layers, simple snacks, charged ID-approved calculator if allowed.
Mindset cue: The exam is a sequence of solvable vignettes. Execute your routine, trust your rules, and keep moving.
References & Further Reading
- USMLE®. Prepare for Your Exam (exam structure, content outline, timing).
- NBME®. Practice & Self-Assessment (forms and score interpretation resources).
- Cepeda NJ, Pashler H, Vul E, et al. Distributed practice in verbal recall tasks. Psychol Sci. 2006. (Spacing effect).
- Roediger HL, Karpicke JD. Test-enhanced learning. J Educ Psychol. 2006. (Testing effect).
- Sweller J. Cognitive load during problem solving. Cogn Sci. 1988. (Cognitive load theory).
- Taylor K, Rohrer D. The effects of interleaving. Appl Cogn Psychol. 2010. (Interleaving benefits).